Photographs by Jennifer Rosenberg
In March 2020, the COVID-19 pandemic changed everyone’s lives nearly overnight, and doctors and nurses have borne the brunt of that upheaval. They’ve endured fear, uncertainty, exhaustion, loneliness, and grief as they cared for patients who were not only profoundly sick but also alone. Now, a year into the pandemic, Northshore magazine is honored to hear from some of our local healthcare heroes.
Joe Cartier, RN
Telemetry Nurse, Anna Jaques Hospital
“It’s like gearing up for a war, basically. You don’t know what you’re fighting, and you don’t know what you have for weapons to fight it, but you have to fight it.”
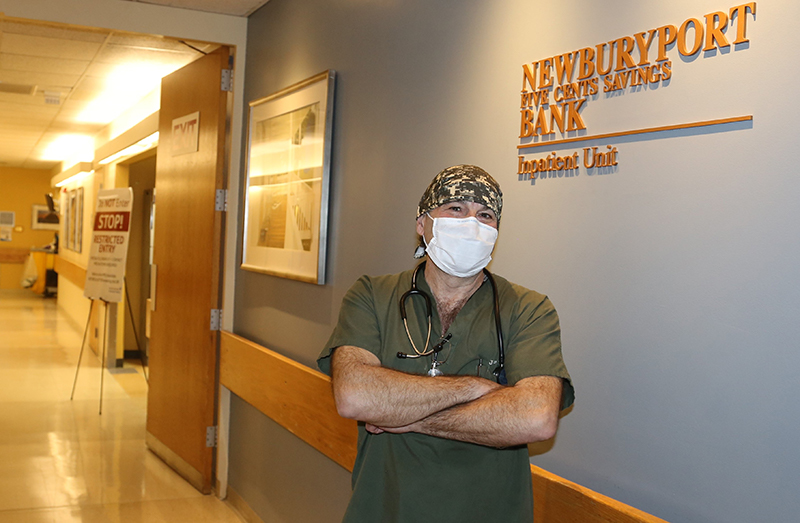
“Seeing people that lose the battle with COVID…they die alone, basically. I’ve seen many people die alone. It’s just sad. It really breaks your heart. There’s nothing you can do, nothing they can do. It’s emotionally wrenching. I’d tell people to be smart with your masks. The more you prevent the spread of COVID, the easier my job’s going to be. Everyone be patient. Work together, we’ll get through this. It’s just a matter of time.”
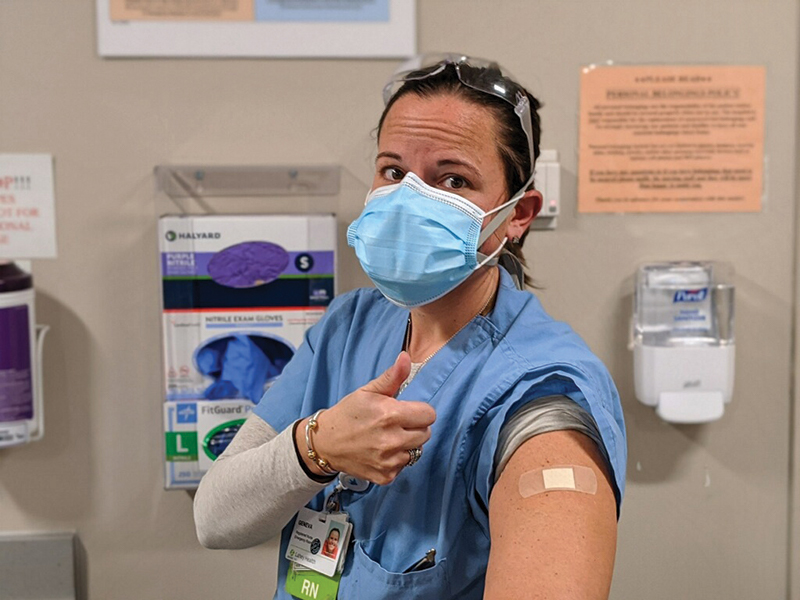
Megan Staples, BSN, RN
Team Lead in the Critical Care Unit, Beverly Hospital
“I don’t want my community to go through what I’ve seen my patients go through and so I want to be kind of a beacon of hope by getting the vaccine myself and showing that it’s safe and that I believe in science.”

“My husband and I actually ended up contracting COVID in May and we had the longer-term side effects. I feel like before COVID I was able to really have a good work-life balance. I could leave work and have my day off and come back to work fresh. But I found that the line between work and being home was blurred because when I was home I felt guilty that I wasn’t at work helping, or I felt concern for my coworkers and the fatigue that they were experiencing. The most challenging part for us was the fact that we had to fill the emotional void of a no-visitor policy. Patients were alone, they were scared, they were in our unit for weeks. They longed for human contact.”
Dermot Lahey, ACNP-BC
Emergency Room Nurse Practitioner, Winchester Hospital, and the first employee at Winchester Hospital to receive the COVID-19 vaccine
“People ask me, did you have any side effects? I said yes, I had one major side effect: Hope.”

“I think one of the big misconceptions that people have is [believing] it’s so risky to get this vaccine because it’s so new. And I’ll say, you know what’s definitely risky? Getting COVID. Sure, you might come through the infection fine, and then in a month, you might come in because you’ve had a stroke, or because of what COVID can do to your blood clotting cascade, or you can have permanent lung damage. I would say those are very real risks, and the risks of being vaccinated pale in comparison to what COVID is. Sometimes people get focused on these tiny little details, and I would say, let’s look at the big picture and refocus on what it is that you’re afraid of.”
Peter Sebeny, MD, MPH
Infectious Disease Physician and Medical Director of Infection Prevention, Anna Jaques Hospital
“I have a background internationally in emerging diseases and epidemiology and we always knew a pandemic was possible, but this one really caught us off guard.”

“I remember [after] some of our first patients recovered after a very long, arduous hospitalization—I’m talking 30, 50 days in the hospital—we did a “Code Happy” where we would play the Pharell song “Happy,” and the nurses and doctors would line up socially distanced outside as the patient’s being discharged to rehab and we would cheer them on.
“Another bright spot is getting vaccinated. That’s the game changer. Getting vaccinated and having vaccine acceptance rates high is really the only way to begin to end the pandemic. I did it for my own health, for that of my family, but also it’s your duty to do this as a personal responsibility as a citizen. We’re all at risk. We do this for ourselves, but we also do it for the greater good.”
Geneva Flowers, RN
Emergency Room Nurse, Beverly
“It’s everywhere. It’s everywhere and you can never let your guard down.”
“I never used to walk into work scared of what we would face until this started. It’s a little bit of being fearful of what you’re going to face in terms of: How sick are the patients going to be today? Are you going to be more short-staffed because some of your co-workers are getting sick now? Are we going to have enough beds in the hospital for all the patients or are we going to have to coordinate more transfers? But also just: Am I going to be exposed today? Am I going to expose my family today? Is today that day?
“It isn’t just the physical demands anymore. Being on my feet for 12 hours is easy. It’s the emotional weight, the calling the family members and saying your loved one’s corona swab came back positive and them being blown away by it, by the idea of what that means going forward. And do they have to go get tested? Who do they have to call? That’s what is really heavy. And in addition, having to constantly tell them I understand that your loved one is in the hospital and no, you can’t come see them.”
Barbara Green, MS, RN, CEN
Emergency Room Nurse, Anna Jaques Hospital
“It’s really unlike anything else that’s happened during my 26 years of nursing.”

“We have things that we do with emergency response, like code situations, and normally we would rush right into the room and be ready to go right now. But there was that short pause where we had to take a really important moment to put on all of our [PPE] gear before we rushed into the room. That is one of the biggest struggles for any ER doctor or nurse, I can tell you that. If this person needs chest compressions we want to do it this second and not 15 seconds later.
“One of the most poignant things that happened was [after] a grueling day, there were five or six mothers with their children, all spread out on the front walk where we exit the building, and they were holding posters that said things like, ‘We’re here for you.’ That was really touching.”
Karen Keaney, MPAH, RN, ACHCE
Associate Chief Nursing Officer, Emergency Services and Case Management, Winchester Hospital
“To be on the front lines, I think there was a level of fear that people had never experienced before and I do think this team faced it head on.”

“The one luxury [healthcare workers] have—and it might be the only luxury we have—is that none of us are isolated like many people in our communities are. So we’re fortunate. We have each other. We have a little bit more normalcy compared to other people, so I guess that’s a little bit of a bright spot. At least we can come in and talk to each other and sort of work through our challenges as a team and then get on with our days here.”
“I think most people who have worked in the trenches over the past 10 months are not hesitant at all to get immunized. I was actually pretty emotional. Not so much for me, but just what it symbolized. My hope is truly that it is the beginning of the end.”

